

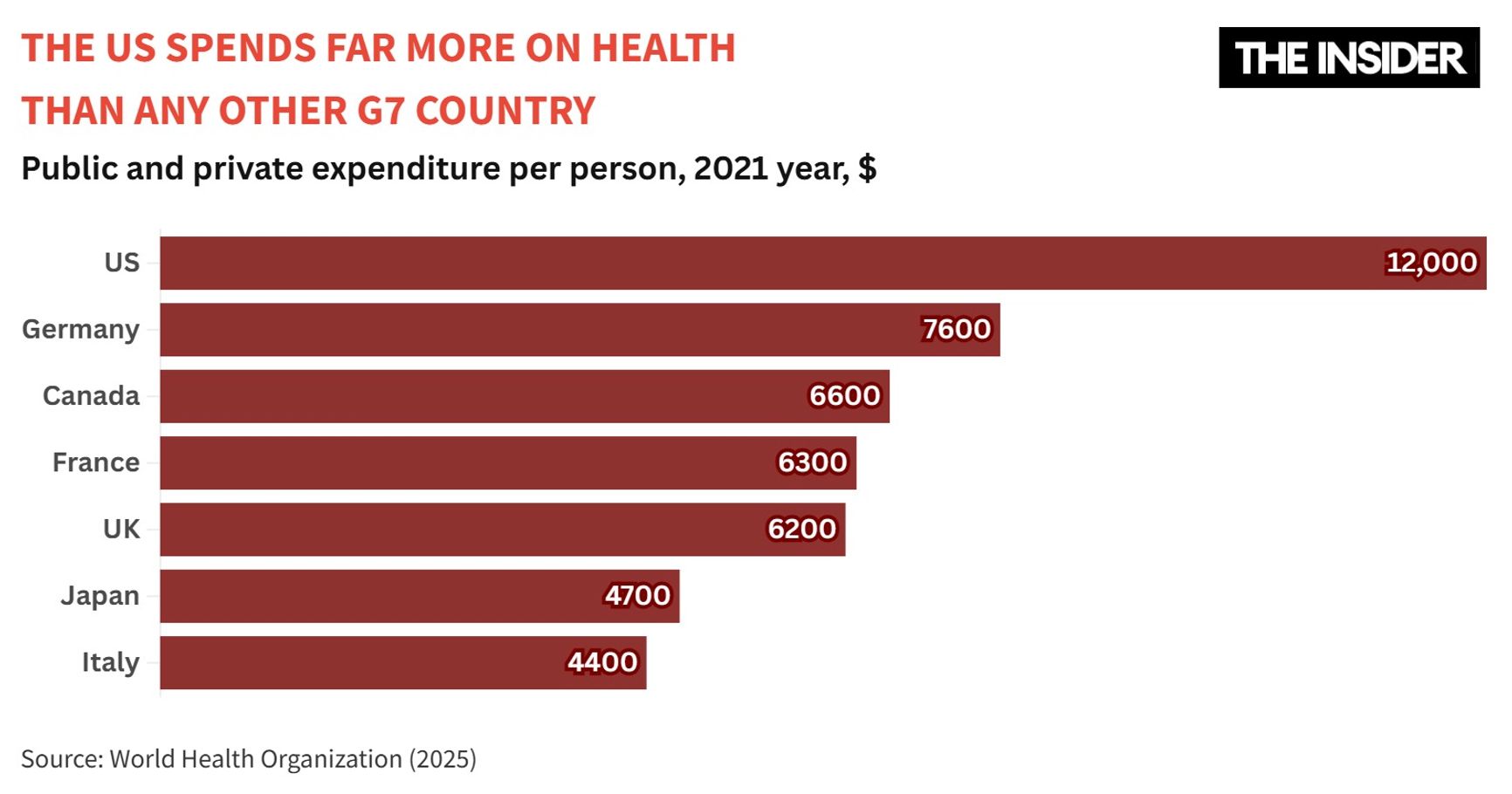
The United States spends more on healthcare than any other G7 country, according to a March study by the Our World in Data project. Yet among G7 nations, the U.S. ranks last in life expectancy and lags behind on most other health indicators. Healthcare has long been a central issue in American politics, and the debate only intensified after Luigi Maggione, outraged by the system’s injustices, killed a top executive of the country’s largest health insurance company. Amid the uproar, Donald Trump vowed to fix America’s “inefficient” healthcare system. So far, however, his only proposal has been to make medical service prices more transparent, a measure that experts argue will do little to improve healthcare accessibility. The root of the problem is far deeper: the U.S. is the only developed country without universal government health insurance. Not only does Trump oppose introducing such a system, but he even tried to repeal its weaker alternative — Obamacare — which had greatly increased the number of insured Americans. Meanwhile, about a third of Americans are forced to forgo necessary medications due to costs.
Content
The sickest among the wealthy
The downsides of private insurance
Inefficient spending
What Trump plans to do
“Making America Healthy Again by Empowering Patients with Clear, Accurate, And Actionable Healthcare Pricing Information” — this is the title of an executive order signed by Donald Trump in late February. The order directs federal agencies to develop, within 90 days, a mechanism for disclosing actual, rather than estimated, prices for hospital and insurance services. In essence, the new directive is meant to reinforce the “Improving Price and Quality Transparency in American Healthcare” order, which Trump signed in 2019 during his previous term. That order required hospitals to publish detailed, user-friendly price lists and mandated that insurers disclose negotiated rates with providers while also delivering discounted prices for prescription drugs.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
“You're not allowed to even talk about it when you're going to a hospital or see a doctor. And this allows you to go out and talk about it,” Trump told reporters at the signing. “It's been unpopular in some circles because people make less money, but it's great for the patient.”
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.

President Donald Trump addresses journalists before signing a decree on healthcare pricing.
In reality, however, the systemic problems of American healthcare are far too deep for this executive order — or any other — to root out. The issue lies not in specific regulations, but in the very foundation of the system itself.
The sickest among the wealthy
The United States is the richest country in the world, but far from the healthiest. Over the past 40 years, the U.S. has fallen far behind other developed nations in life expectancy. In 1980, the gap was less than a year (73.7 vs. 74.6), but by the early 2020s, it had widened to more than four years (78.4 vs. 82.5). Despite having the highest healthcare spending among developed countries, the U.S. has the lowest life expectancy for both men and women.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
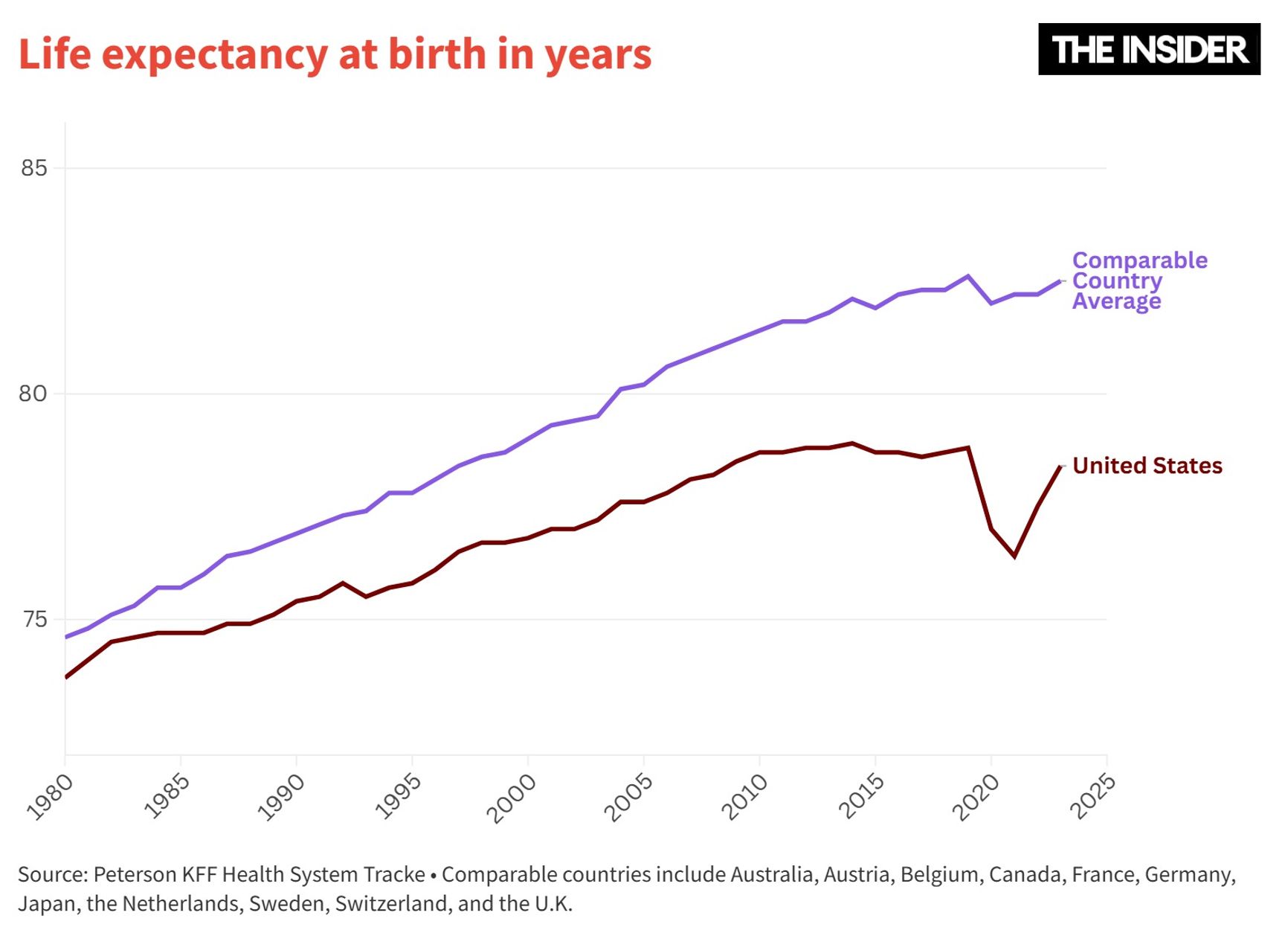
Among all U.S. states, Hawaii leads in life expectancy at birth, with an average of 79.9 years. Yet even this figure is lower than in most OECD countries. The number of deaths that could have been prevented with timely medical intervention is also significantly higher in the U.S. (368 per 100,000 people) than in other developed nations. In Germany, for example, this figure is 194 per 100,000, while in Switzerland it is just 131. Even in U.S. states with relatively low rates of preventable mortality — such as Minnesota, Utah, Massachusetts, and Connecticut — the numbers remain above the international average.
Wealthier Americans live 10 to 15 years longer than the poorest, and rather than mitigating these disparities, the healthcare system often exacerbates them. Yet even the most privileged Americans have worse health outcomes compared to citizens of other developed nations.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
Wealthier Americans live 10 to 15 years longer than the poorest, and rather than mitigating these disparities, the healthcare system often exacerbates them
Why can’t even the most progressive U.S. states overtake the majority of developed countries, which, after all, spend far less on healthcare?
The downsides of private insurance
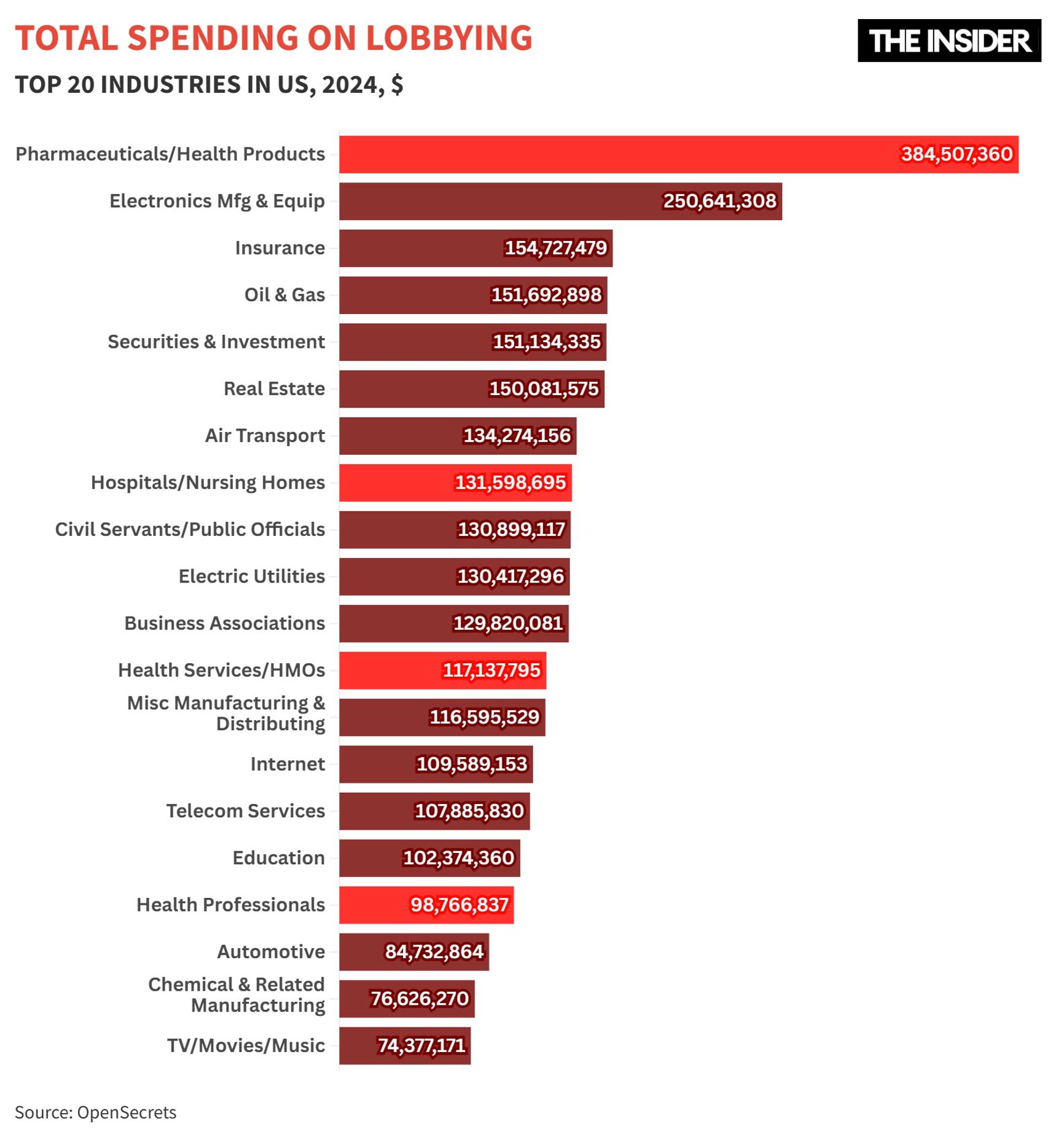
The biggest problem with the U.S. healthcare system is its very structure, which relies on private insurance companies. Since the mid-20th century, the American Medical Association has opposed government-run health insurance. All industry players had a vested interest in maintaining a system in which hospitals and pharmaceutical companies set their own prices, while insurers shifted the costs onto employers.
As a compromise, the Medicare and Medicaid programs were introduced in 1965 to provide coverage for those without access to private insurance. But three decades later, medical and insurance companies once again joined forces to block healthcare reform efforts under President Bill Clinton.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
Since the mid-20th century, the American Medical Association has opposed government-run health insurance
Under Barack Obama, the U.S. saw its most ambitious healthcare reform since the 1960s. The “Patient Protection and Affordable Care Act,” better known as “Obamacare,” was signed into law in 2010. It required uninsured Americans to purchase health insurance while offering subsidies for low-income individuals. Employers and insurers were prohibited from denying coverage or increasing premiums for employees based on pre-existing and chronic conditions.
By 2016, this reform had nearly halved the percentage of uninsured Americans. However, it did not solve all systemic issues, especially since some key provisions were only implemented years after the law went into effect. During his first term, Donald Trump came close to repealing the law entirely.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
While most developed countries provide universal government health coverage, about 8% of the U.S. population — 27 million people — remain uninsured. According to a Gallup survey, in 2022, 38% of Americans avoided medical care due to its high cost — and 27% of these faced serious health issues.
In 2024, around 14 million Americans owed more than $1,000 for medical services they had already received, while 3 million had medical debt exceeding $10,000.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
Nearly 40% of Americans avoid going to the doctor due to high costs
Medical expenses can be overwhelming even for insured patients. In Minnesota — one of the top states in terms of healthcare quality — the average annual insurance cost is $2,700, roughly 6% of the median local income.
Inefficient spending
According to a Health Affairs study, 25% to 50% of all U.S. healthcare spending is wasted — i.e. it constitutes money spent without improving public health. This includes payments for procedures with no proven clinical effectiveness, such as unnecessary surgeries for minor lower back pain or early labor induction in low-risk pregnancies.
Administrative expenses — such as billing, insurance paperwork, and record-keeping — account for 15–30% of total U.S. healthcare costs. This is twice the amount spent on the treatment of cardiovascular disease and three times the amount spent on cancer care.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
Administrative costs in the U.S. healthcare system are three times higher than outlays on cancer treatment
For ordinary Americans, the biggest burden is high prices. The cost of the same medical service varies widely not only between the U.S. and other countries, but also among different states. The most striking differences are in drug prices. Even when adjusted for purchasing power parity, healthcare in the U.S. remains far more expensive than the OECD average.
Several factors contribute to this disparity. One of the key issues is the lack of a unified negotiator. In most countries, drug prices are set through negotiations with a single central authority, such as the government. In the U.S., however, thousands of separate buyers negotiate with pharmaceutical companies, weakening their bargaining power. In 2022, the Inflation Reduction Act allowed the Medicare program to negotiate directly with pharmaceutical companies on the prices of certain drugs. But this measure alone is not enough to bring costs down significantly.
Many countries legally cap drug prices. In France, for example, pharmaceutical companies sign contracts with the government that specify both the price and the expected sales volume of new medications. If sales exceed the agreed-upon threshold, manufacturers must refund 50–80% of the excess revenue. This regulation prevents the market from being flooded with expensive drugs not covered by insurance. In the U.S., no such restrictions exist.
When a new drug enters the market, pharmaceutical companies worldwide receive patents, granting them temporary monopolies and preventing the sale of cheaper alternatives. However, U.S. law contains loopholes that allow manufacturers to extend their monopolies by filing new patents that are only indirectly related to the original drug.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.
U.S. law contains loopholes that allow pharmaceutical companies to maintain monopolies on their drugs for years
For example, biosimilars of AbbVie’s Humira entered the U.S. market four years later than in Europe. Patents played a decisive role: the company filed 311 patent applications, of which 165 were approved. From 2016 to 2023, AbbVie earned $114 billion from Humira sales, while the drug's price rose by 60%, reaching $5,007 per vial (40 mg) by the end of 2022.
What Trump plans to do
After Trump’s 2019 price transparency order, clinics and insurers fought in court for the right not to disclose pricing information. Others sabotaged the process, with some providers listing prices on their websites in a way that made them unreadable by search engines. Trump's first-term pledge to lower medical costs ultimately failed. However, his new administration now hopes that the latest executive order will reduce employers’ major healthcare expenses by an average of 27%.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.

New York’s Langone Hospital was one of the institutions that concealed pricing information from search engines
“While price transparency may not fully transform the U.S. healthcare market, it could help both medical providers and patients align expectations on rates,” note McKinsey analysts, who note that prices for the same medical procedures can vary by 40–50%, even within a single state. According to researchers from the University of Chicago’s Booth School of Business, revealing healthcare prices could lead to a 5–7% reduction. And with annual healthcare costs in the U.S. approaching $5 trillion, this could result in savings of approximately $350 billion.
The Organization for Economic Cooperation and Development includes 38 countries, including most EU countries, as well as the U.S., Australia, UK, Israel, Iceland, Canada, Colombia, Costa Rica, Mexico, New Zealand, Norway, Republic of Korea, Turkey, Chile, Switzerland, and Japan.
Exchange rate that takes into account the price level in different economies; determined based on the equality of the cost of a basket of goods and services, calculated in the prices and currencies of the economies being compared.